What is Fatty Liver and Why is it Important in Bariatrics?
Fatty liver disease is a common condition linked to obesity, often developing silently without noticeable symptoms. Recently renamed metabolic dysfunction–associated steatotic liver disease (MASLD), this condition affects roughly one in three adults worldwide and is especially prevalent among people with type 2 diabetes or severe obesity.1 (It used to be called nonalcoholic fatty liver disease, or NAFLD.)
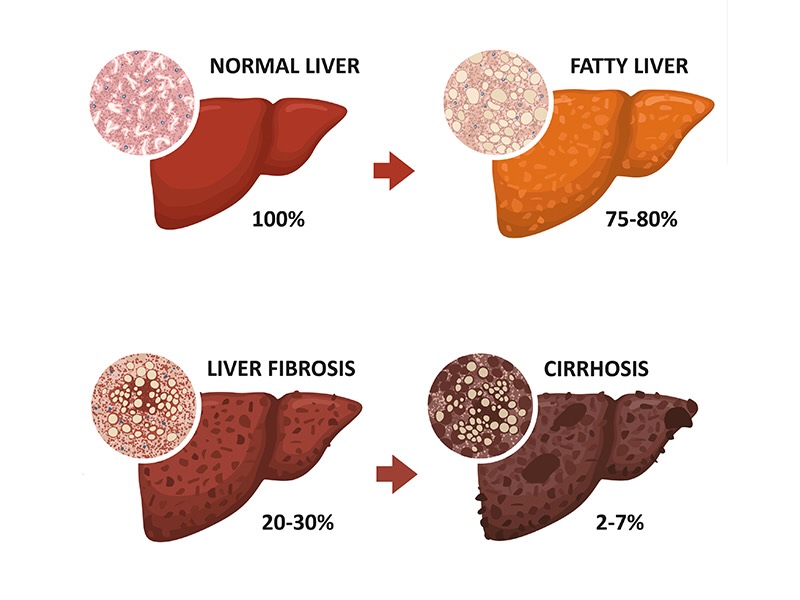
It begins with fat accumulation inside liver cells but doesn’t immediately disrupt function. The liver can adapt for a time, but in about 10–20% of cases, inflammation worsens, progressing to metabolic dysfunction–associated steatohepatitis (MASH). As the body attempts to repair the damage, scar tissue forms (fibrosis). Advanced scarring, or cirrhosis, can reshape the liver entirely and raise the risk of liver cancer.2
What does this mean for bariatric patients? Excess fat in the liver can complicate surgery and recovery, but it’s also a signal of underlying metabolic dysfunction that affects the whole body.
To learn more about fatty liver disease, including the connection to metabolic disease, the cardiovascular system, and gastrointestinal tract, as well as your risk profile, click here.
The encouraging news is that weight loss through lifestyle changes and bariatric surgery can significantly improve liver function, reduce inflammation, and even reverse early scarring. But you have to be proactive and catch it before it progresses too far.